An Interview With Kaley Day

Nearly one year after COVID-19 changed our world and impacted lives globally, the release of two FDA-approved vaccines has offered hope to many. For Colorado’s intellectual and developmental disability community, the relief offered by the vaccine has become imperative to a population more impacted by social isolation, where the function of essential services and supports has changed, and many live with co-occurring or underlying conditions. In these interviews, AdvocacyDenver seeks to understand the development of Colorado’s vaccine priority schedule, along with the perspective of advocates and family members.

What kind of discussion is taking place in the statewide advocacy community around vaccine distribution?
There is ongoing discussion in terms of priorities and where individuals with intellectual and developmental disabilities, and the larger community of individuals with significant health impairments, fall in line as the vaccine is phased in. All of the Arc chapters have launched awareness campaigns. We want self-advocates, parents and providers to have information, in people-friendly terms, in order to make an informed decision in relation to the vaccine. Several of The Arc Chapters, Community Centered Boards, and other disability groups have volunteered with the state to help with vaccine distributions as resources become more plentiful. This collaboration may potentially help with targeted outreach and assist with getting “shots in arms” by trusted providers with whom people have relationships. Collectively, we are excited about the opportunity; however, timing still remains a question. The Governor’s Medical Advisory Committee, The Colorado National Guard, and the Department of Health Care Policy and Financing will continue dialogue as new information becomes available, as Center for Disease Control (“CDC”) guidance evolves, and as vaccines become more abundant. Together, we have been successful in prioritizing individuals that have difficulty wearing masks and adding Down Syndrome to the priority list.
What are the major areas of concern for advocates looking forward?
In many respects, the plane has taken off and we do not have a flight plan. The flight plan is dependent on so many factors. Vaccine availability is limited and variable week-to-week, the logistics of getting vaccines out given the ultra-cold temperatures required, different systems for signing up, the vast geography of the state, communication and transportation challenges in getting to vaccination sites. The world, and Colorado, has never deployed a vaccination distribution scheme on the scale and scope that we see today. A major challenge is that when the vaccine is offered, some individuals decline the resource. We are all looking forward to a world where the majority of our communities are vaccinated to achieve “herd immunity.” Although specific conditions are called out in the priority schedule, we look forward to a schedule that incorporates settings, the ability or lack of ability to social distance, and a more inclusive definition of Intellectual and Developmental Disability (“I/DD”).
Are there any recommendations being made by advocates in regards to the re-opening of in-person services and client safety?
As the pandemic stretches into the coming months, several changes have been made in the waiver programs to offer one-on-one services in lieu of congregate services. This is a protective factor for many people and the flexibility of providing services are an important change. Social isolation and the challenges associated with limited opportunities are top of mind for advocates statewide.

From the larger community, there seems to be a disconnect in understanding why those with intellectual and developmental disabilities should receive priority in the vaccine schedule. As a parent, can you speak to the importance of that priority for your son in particular?
I have a 17-year-old son; his name is Kennedy. Kennedy has Down syndrome and obstructive sleep apnea. It’s terrifying to think as a parent that he wouldn’t receive highest priority, to think of him in a hospital room with very poor outcomes at a potential greater than the average person in the population. There’s a university of Oxford study that looked at 8 million adults in England and identified that people like my son have four to five times the risk of very severe COVID versus the average person in that population, and also a 10 times greater risk of death. The way they’ve done the priorities they think they’ve captured my son and others, but they haven’t. If you look at “1B.3”, while Down syndrome is listed as a condition, in 1B.3 you have to have two conditions. Well, most people with Down syndrome don’t have cancer. They don’t have kidney disease. They don’t have sickle cell anemia. They don’t have organ transplants. Those are all pretty specific singular conditions, and most people with Down syndrome have a range of conditions that aren’t listed there- from obstructive sleep apnea to respiratory issues and compromised immune systems.
The other thing they try to point to is that people with disabilities have difficulty wearing masks. Well guess what? Most people with intellectual and development disabilities really don’t have difficulty wearing masks. My son doesn’t have difficulty wearing a mask. So as it turns out, Kennedy would be in Phase 2 after me. I’m a relatively healthy 65-year-old who plays tennis and walks, but my son, who’s a greater risk than me is prioritized after me. I would like to see is equity and parity for my son and others. There have been over one million people prioritized. Our population of adults (with intellectual and developmental disabilities) is maybe 10- to 20,000, so over a million have been prioritized, and somehow Kennedy is in Phase 2. Most people with intellectual and developmental disabilities, are in Phase 3. They’re in Phase 3 because they don’t have difficulty wearing masks, they don’t have Down syndrome, and they don’t have the very specific conditions listed in 1B.3 and 1B.2. So while the state thinks they’ve addressed this, they haven’t, and they put people like my son at risk.
How has Kennedy and your family’s life been affected by both the pandemic and its risks, as well as this delay in vaccination and getting back to the community?
Kennedy is extremely social. He’s a hugging machine for one thing, so the only people that he can hug now are people in the house. His ability to get together socially with his friends and schoolmates is drastically limited. If he were 18 his ability to be employed would be greatly impacted. The ability to go out and have birthday parties, go out to Chuck E Cheese and Red Robin, all of that’s been severely impacted. Those are things that are very meaningful in his life. Not the least of which is school, where his typical classmates are hybrid, so he doesn’t get to see them and he has difficulty with remote learning. He’s not contracted COVID, but he’s been in quarantine two or three times because others have.
As a parent, what action would you urge state officials to take in response to these concerns?
They have Down syndrome in 1B.3 and they have “PWD” (people with disabilities) who have difficulty with wearing masks. Just call it “PWD” or call it people with intellectual and developmental disabilities. What is the harm in going the extra distance? Spell out our population who is probably more severely impacted, or as severely impacted as anyone else, to resume more of a normal life. What’s the harm in doing that? It’s a small population. I don’t understand why this is such a struggle with HCPF, CDPHE, and the governor’s office. I don’t understand.
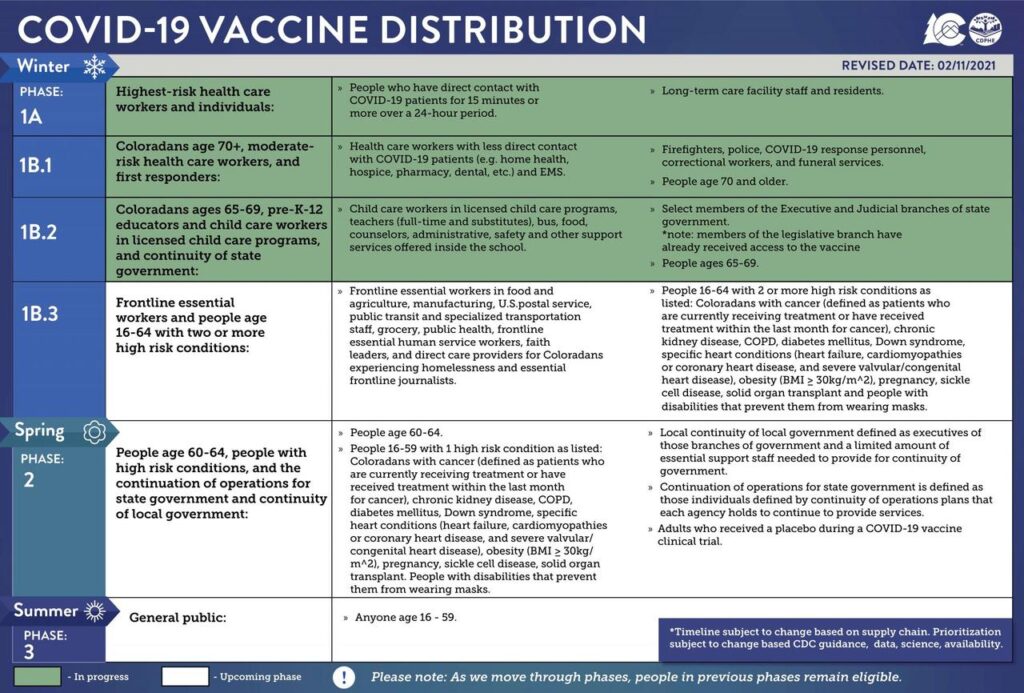
Colorado’s current vaccine distribution schedule is available here

Apart from the addition of Down syndrome to Phase 1B.3, what considerations are being discussed in Governor’s office in regards to the vaccine priority schedule and people with disabilities?
Josh Winkler: As you’ve already seen, things change. The original phasing came out in early January with very limited knowledge of what the Centers for Disease Control (“CDC”) was putting out and how many doses a state would be getting per week. There’s been a couple of revisions since, including about two weeks ago when Down syndrome was added. The 1B.1, 1B.2, and 1B.3 categories were all added, and those were largely based on CDC guidance, and revisions to that guidance, which included Down syndrome in particular as one of the conditions that data has shown has a correlation between mortality and that underlying condition.
All of those conditions [in those categories] are the same. Those are the conditions the CDC has found strong, scientific evidence that there’s a correlation. So at any given time the CDC could upgrade their recommendations. As we get changes on dosing, or another vaccine is approved- all those things could influence when there’s more revisions to the phasing. Nothing is set in stone. There’s a whole team of epidemiologists and doctors that are reviewing all of the information. We are trying to balance out the recommendations from the CDC and the numerous groups that are lobbying for why they think they should be moved higher in the priority, making sure that there’s a prioritization that preserves life and understanding how many doses we have coming into the state. Ideally we vaccinate everybody as quickly as possible, but we still only get about 100,000 doses a week at this point.
In terms of disability, how is that being defined? Is it like the Rehabilitation Act that defines a disability as a physical or mental impairment that significantly limits a major life activity?
Josh Winkler: Unlike a lot of other states, we haven’t gone with that broad of language. Again, it’s been that balance of going specific and calling out the specific things the CDC has identified as underlying conditions, and being broad enough that you’re not missing somebody who has some kind of rare disorder that’s very similar to, but not quite, the exact label. Rather than saying ‘intellectual and developmental disabilities’, for example- that’s not really what the evidence has shown there’s been the correlation of death with. It’s the underlying conditions that many people with I/DD might have. So if somebody has a heart condition and I/DD, they could be in that category because it’s the heart condition that puts them at a higher risk based on the CDC data.
Is there any current or projected data around COVID-19 incidence or cases in Colorado’s community of individuals with disabilities?
Bonnie Silva: We have two pieces of data around COVID that are specific to people with disabilities. Early on, Colorado realized that people with disabilities and older adults residing in congregate settings would be disproportionately impacted by this pandemic, so we immediately began tracking data specific to those settings to understand where the impact was the most significant and how to deploy our resources to mitigate the spread of COVID and to save lives. There’s also the data that HCPF has for people who reside in home- and community-based waivers, so not those in group congregate settings, but in community-based programs. So you would ask, ‘what does that data show us?’ Our data shows that people who reside in high-density group settings are at high risk for poor data outcomes from COVID. We also see that age in the disability population, similar to the non-disability population, is a high correlating factor for death.
First and foremost, hats off to the people of Colorado, because what our data shows is that people with disabilities who received services in Colorado are at a fairly low risk for mortality from COVID. That means they have done a good job with social distancing and adhering to the infection prevention guidelines that are out there. How this community has shown up and our data is not necessarily replicated in other states. I think it’s something that we, as a community, should be very proud of.
When looking at those group settings, by far people in nursing homes have been the most impacted, followed by people who reside in assisted living residences, then followed by group homes serving people with I/DD. More specifically, it’s 23% of the deaths have been from people in nursing homes, followed by 10.7% in assisted living, and 0.1% for the group homes serving people with I/DD. Of course all of those deaths are tragic, but we’ve worked hard to make sure that, on the prevention side, we take this holistic approach. We didn’t separate out a response for a nursing home from a response for people serving I/DD, we provided the same level of support across the board. Group homes are licensed to serve around eight to 10 people, whereas a nursing home might have 200 beds, so there’s a pretty big continuum when talking about group settings. We very intentionally included all of these early on in our holistic response and I think our data supports the outcomes for that.
In which of those three data sets would the state regional centers, for example Wheat Ridge Regional Center, fall?
Bonnie Silva: In the group home category, so that 0.1% group.
In terms of people in the community, the adult waivers serving people with I/DD had the lowest mortality rate when we’re looking at cross-disability population. That rate would increase when we look at, for example, the Elderly, Blind, and Disabled waiver, where we’re serving more older adults than we are in the I/DD waivers. If you’re looking for where the concentrated risk is, it’s the combined factors of disability, age, and setting that was the greatest risk for people.
Josh Winkler: One thing that surprised me on the data was that the general Medicaid population actually saw that deaths were at twice the rate of what they were in the waivers. So of the deaths in the general Medicaid population, twice as many were from COVID as the deaths in any of the waivers. Again, it goes to show how in-home care and people on Home and Community Based (“HCBS”) waivers in Colorado have done a great job of staying home, practicing social distancing, and wearing masks.
Looking at service providers and the future of service provision in the state, what expectations or recommendations are being made to service providers regarding the vaccine?
Bonnie Silva: Colorado made the decision, in terms of priority, to make sure that the direct support professionals providing care to people with disabilities were in that top-tier priority. If they provided care in group homes, they were in Phase 1A. If they provided in-home care to people on waivers, they were in that 1B.1 category. While there’s a lot of hope on the horizon in terms of vaccines finally being deployed, we need to have a good percentage of Colorado vaccinated in order to reach that “herd immunity.”
What we know is that the vaccine doesn’t necessarily stop the spread of COVID. It stops people from dying from COVID if they get it. I imagine for some time, at least at this juncture, that the infection prevention measures we have in place now will need to remain in place- the smaller group delivery of services, wearing masks, hand washing, social distancing- until we have a much larger percentage of the Colorado population vaccinated.
What discussion or planning is in place should a provider or a client refuse the vaccine? Is there an expectation from the state around disclosure from service providers in regards to whether they receive the vaccine or not?
Bonnie Silva: Vaccine confidence has been one of our key strategies that’ we’ve been working across trade provider organizations. We’ve hosted several Q&As to help people get trusted information in a way that helps them to make informed decisions. I know many of the trade organizations, in addition to the state efforts, are hosting their own campaigns to help the direct care providers, as well as members, understand the vaccine. There’s so much misinformation out there, so we’re working really hard to give people informed information to make solid decisions. That said, there’s no plans for us to require providers or members to take the vaccine or disclose whether or not they’ve taken the vaccine, at least not at this juncture. That might be something in the future to consider, but at this point we have seen that staff are pretty forthcoming about their willingness. We must continue to have those infection prevention plans in place because we don’t have vaccine acceptance across the board.
With the initial rollout of the vaccine in December, we had what I think we all found to be a fairly disheartening level of acceptance for the vaccine. Now here we are in February and it’s jumped leaps and bounds by 25-30%. We are hopeful that those acceptance rates will continue to jump up significantly in the coming months.
Josh Winkler: I would add that you don’t lose eligibility if you didn’t get it when you first became eligible. So whether that was residents or employees in a facility, they’re still eligible. When we move on to Phase 2 everybody in Phase 1A and the 1B categories will still be eligible. It’s a good thing but also adds to the need to err on the side of caution when we are figuring out the numbers on how far the doses will go and how long it’ll take to get through a phase.
Bonnie Silva: Our biggest constraint right now is the federal supply of the vaccine. We are ready! Give it to us, federal government, and we will deploy! We are all anxiously awaiting the day that any Coloradoan who wants a vaccine will be able to get one. Our biggest challenge right now is that we simply don’t have enough vaccine coming in.

Kaley Day is an Advocate for Adults with AdvocacyDenver.
She is a graduate of the University of Denver, majoring in Strategic Communication, and a sibling to a young man with disabilities. Kaley publishes Policy Perspective featuring interviews with state policymakers and community members on issues that affect the work and mission of AdvocacyDenver.
For questions or comments, contact Kaley at kday@advocacydenver.org